Mon - Saturday, 09:00 AM - 07:00 PM
Mon - Saturday, 09:00 AM - 07:00 PM

Screening tests can help find cancer at an early stage, before symptoms appear. When abnormal tissue or cancer is found early, it may be easier to treat or cure. By the time symptoms appear, the cancer may have grown and spread. This can make the cancer harder to treat or cure. It is important to remember that when your doctor suggests a screening test, it does not always mean he or she thinks you have cancer. Screening tests are done when you have no cancer symptoms.
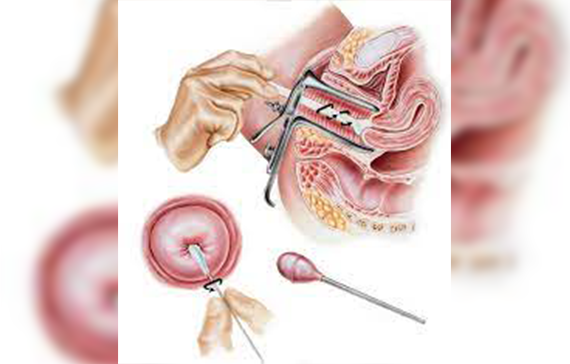
Human papillomavirus (HPV) testing
Cells are scraped from the outside of a woman’s cervix. These cells are tested for specific strains of HPV. Some strains of HPV are more strongly linked to an increased risk of cervical cancer. This test may be done alone or combined with a Pap test (see below). An HPV test may also be done on a sample of cells from a woman’s vagina that she can collect herself.
Pap test
This test also uses cells from the outside of a woman's cervix. A pathologist then identifies any precancerous or cancerous cells. A Pap test may be combined with HPV testing.
Visual inspection with acetic acid (VIA)
VIA is a screening test that can be done with a few tools and the naked eye. During VIA, a dilution of white vinegar is applied to the cervix.
The health care provider then looks for abnormalities on the cervix, which will turn white when exposed to vinegar. This screening test is very useful in places where access to medical care is limited.
The treatment of cervical cancer depends on several factors, including the type and stage of cancer, possible side effects, and the patient’s preferences and overall health. Take time to learn about all of your treatment options and be sure to ask questions about things that are unclear. Talk with your doctor about the goals of each treatment and what you can expect while receiving the treatment. These types of talks are called “shared decision making.” Shared decision making is when you and your doctors work together to choose treatments that fit the goals of your care. Shared decision making is particularly important for cervical cancer because there are different treatment options.
Cervical cancer treatment.......There are different types of treatment for patients with cervical cancer.
Five types of standard treatment are used:
Five types of standard treatment are used:
Surgery
Surgery (removing the cancer in an operation) is sometimes used to treat cervical cancer. The following surgical procedures may be used:
Conization:
A procedure to remove a cone-shaped piece of tissue from the cervix and cervical canal. A pathologist views the tissue under a microscope to look for cancer cells.
Conization
may be used to diagnose or treat a cervical condition. This procedure is also called a cone biopsy.
Conization may be done using one of the following procedures:
Cold-knife conization: A surgical procedure that uses a scalpel (sharp knife) to remove abnormal tissue or cancer.
Loop electrosurgical excision procedure (LEEP)
A surgical procedure that uses electrical current passed through a thin wire loop as a knife to remove abnormal tissue or cancer.
Laser surgery: A surgical procedure that uses a laser beam (a narrow beam of intense light) as a knife to make bloodless cuts in tissue or to remove a surface lesion such as a tumor.
The type of conization procedure used depends on where the cancer cells are in the cervix and the type of cervical cancer.
Hysterectomy
The uterus is surgically removed with or without other organs or tissues. In a total hysterectomy, the uterus and cervix are removed. In a total hysterectomy with salpingo-oophorectomy, (a) the uterus plus one (unilateral) ovary and fallopian tube are removed; or (b) the uterus plus both (bilateral) ovaries and fallopian tubes are removed. In a radical hysterectomy, the uterus, cervix, both ovaries, both fallopian tubes, and nearby tissue are removed. These procedures are done using a low transverse incision or a vertical incision.
Radical hysterectomy
Surgery to remove the uterus, cervix, part of the vagina, and a wide area of ligaments and tissues around these organs. The ovaries, fallopian tubes, or nearby lymph nodes may also be removed.
Modified radical hysterectomy
Surgery to remove the uterus, cervix, upper part of the vagina, and ligaments and tissues that closely surround these organs. Nearby lymph nodes may also be removed. In this type of surgery, not as many tissues and/or organs are removed as in a radical hysterectomy.
Radical trachelectomy
Surgery to remove the cervix, nearby tissue and lymph nodes, and the upper part of the vagina. The uterus and ovaries are not removed.
Bilateral salpingo-oophorectomy Surgery to remove both ovaries and both fallopian tubes.
Pelvic exenteration
Surgery to remove the lower colon, rectum, and bladder. The cervix, vagina, ovaries, and nearby lymph nodes are also removed. Artificial openings (stoma) are made for urine and stool to flow from the body to a collection bag. Plastic surgery may be needed to make an artificial vagina after this operation.
Endometrial cancer begins in the layer of cells that form the lining (endometrium) of the uterus. Endometrial cancer is sometimes called uterine cancer. Other types of cancer can form in the uterus, including uterine sarcoma, but they are much less common than endometrial cancer
Endometrial Cancer Treatment
Specific treatment for endometrial cancer will be determined by your doctor(s) based on:
1-Your overall health and medical history
2-Extent of the disease
3-Your tolerance for specific medications, procedures or therapies
4-Expectations for the course of the disease
5-Your opinion or preference
The choice of treatment depends on the stage of cancer — whether it is only in the endometrium, or if it has spread to other parts of the uterus or body. Most people will be treated with surgery first. Some may need additional therapy. Generally, treatment for people with cancer of the endometrium includes one or more of the following.
Surgery
Hysterectomy — surgical removal of the uterus
Salpingo-oophorectomy — surgery to remove the fallopian tubes and ovaries
Pelvic lymph node dissection — removal of some lymph nodes from the pelvis
Para-aortic lymphadenectomy— removal of lymph nodes that surround the aorta, the main artery of the heart
Laparoscopic lymph node sampling — removal of lymph nodes through a narrow viewing tube called a laparoscope, which is inserted through a small incision (cut) in the abdomen (belly)
Sentinel lymph node mapping — use of fluorescent imaging to identify potentially cancerous lymph nodes that would otherwise go undetected
Radiation therapy
the use of X-rays, gamma rays and charged particles to fight cancer. Brachytherapy and external beam radiation are the most common radiation therapies used to treat endometrial cancer. Novel techniques in image-based brachytherapy with directed magnetic resonance (MR) guidance offer better patient outcomes and fewer side effects.
Chemotherapy the use of anticancer drugs to treat cancerous cells
Immunotherapy the process of activating the immune system’s natural ability to fight cancer
Hormone therapy medication or surgical procedures that interfere with hormone activity
Treatment for ovarian cancer Treatment for ovarian cancer will depend on: the size and type of ovarian cancer you have where the cancer is if it has spread your general health The main treatments are surgery and chemotherapy. Other treatments include targeted medicines and hormone treatments.
Breast cancer most often begins with cells in the milk-producing ducts (invasive ductal carcinoma). Breast cancer may also begin in the glandular tissue called lobules (invasive lobular carcinoma) or in other cells or tissue within the breast.
Signs and symptoms of breast cancer may include:
Mammography
Mammography is a type of x-ray specifically designed to view the breast. The images produced by mammography can show tumors or irregularities in the breast. These images are called mammograms.
Clinical breast examination
A medical professional looks and feels for any changes in the breast’s size or shape. The examiner also looks for changes in the skin of the breasts and nipples.
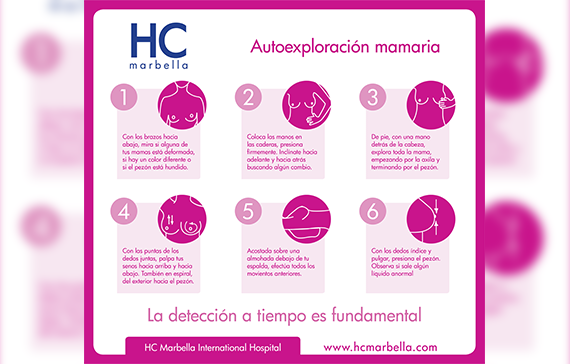
Breast self-examination
During this exam, a woman looks and feels for changes in her own breasts. If she notices any changes, she should see a doctor.
Magnetic resonance imaging (MRI)
An MRI is not regularly used to screen for breast cancer. But it may be helpful for women with a higher risk of breast cancer, those with dense breasts, or when a lump is found during a breast exam.